Table of Contents
Ear, Nose & Throat Examination Notes for Medical Students
THE EAR HISTORY & HEARING TESTS:
The Interview – Ear Related History
- Presenting Symptoms
- Pain,
- Discharge
- Itching,
- Vertigo
- Tinnitis
- Changing in Hearing
- History of Presenting Symptoms
- Onset – weeks day, months
- Contributing factors – trauma, recent illness, exposure to sudden loud noise
- Which ear effected
- Does anything make it worse, does anything make it better.
- Medical History – Note specifically
- Hypoxia at birth
- Low birth weight – less than 1500g
- Congenital abnormalities of the face or skull
- Maternal drug use
- Head trauma
- Ear trauma
- Genetic disease – Meniere’s Disease
- Chronic and acute infections – ear, sinus, colds, flu
- Surgical History – Note specifically
- Ear surgery – grommets etc
- Sinus surgery
- Head and facial surgery
- Nerosugery
- Medications: Many medications can be ototoxic. Note spefically:
- Large doses of Aspirin
- Gentamicin Sulphate
- Aminoglycosides
- Social History – Note specifically:
- Exposure to loud noises at work, availability and us of PPE
- Exposure to Industrial noise
- Exposure to recreational noise
- Family History – Note Specifically
- Family history of hearing loss
- Genetic disorders
EXAMINATION OF THE EAR
External structures:
- Briefly examine the outer structures
- Colour and texture of the skin
- Any moles, cysts, nodes, or deformities
- Any skin changes suggestive of cancer (e.g basal cell, melanoma,
- Any signs of swelling and/or redness
- Discharge – colour and odor
- Palpate the ear for pain, tenderness, skin texture and lesions.
- If pain increases – external ear infection likely
- No pain increase – middle ear infection likely
- Tenderness in mastoid area – possible mastoiditis
External Auditory Canal and Tympanic Membrane:
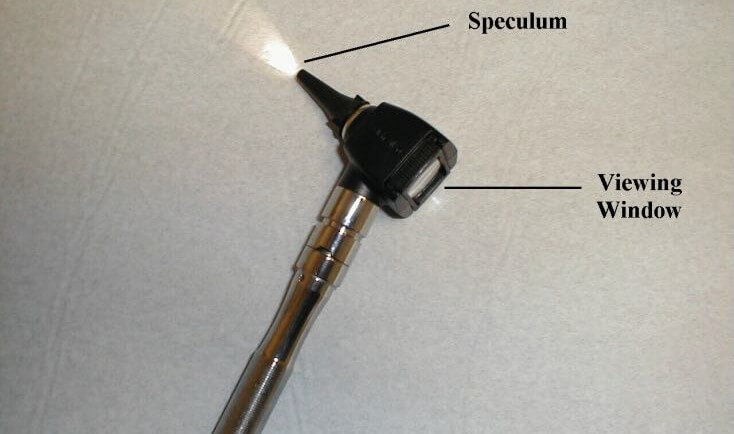
- The Otoscope:
- The otoscope allows you to examine the external canal,, as well as the tympanic membrane and a few inner ear structures. Use the biggest earpiece that can fit in to the ear canal.

Examination procedure:
Always examine the unaffected ear first.
- Place the tip of the specula in the opening of the external canal.
- Gently grasp the top of the left ear with your left hand and pull up and backwards. This straightens out the canal, allowing easier passage of the scope.
- Look through the viewing window with either eye. Slowly advance the scope, heading a bit towards the patient’s nose but without any up or down angle.
- As you advance, pay attention to the appearance of the external canal. In the setting of infection, called otitis externa, the walls becomes red, swollen and may not accommodate the speculum. In the normal state there should be plenty of room.

The Tympanic Membrane:
- The tympanic membrane (a.k.a. ear drum) should be visible. Pay particular attention to:
- The color: When healthy, it has a grayish, translucent appearance.
- The structures behind it: The malleous, one of the bones of the middle ear, touches the drum.

An annulus fibrosus
Lpi long process of incus – sometimes visible through a healthy translucent drum Um umbo – the end of the malleus handle and the centre of the drum
Lr light reflex – antero-inferioirly Lp Lateral process of the malleus
At Attic also known as pars flaccida
Hm handle of the malleus
- In the setting of infection within the middle ear, the drum becomes diffusely red and the light reflex is lost.
- fluid collecting behind the drum. This is called a middle ear effusion and can cause the drum to bulge outwards.
Detecting Conductive v. Sensorineural Deficits:
- Conduction: The passage of sound from outside to the level of the 8th cranial nerve. This includes transmission of sound through the external canal and middle ears.
- Sensorineural: The transmission of sound through the 8th nerve to the brain.
Hearing loss can occur at either level. To determine which is affected, the following tests are performed: Pure tone audiometry is used to measure the softest sounds that a person can hear at different pitches. Speech audiometry is used to assess how well a person can recognize and repeat words at different volumes. These tests help determine the degree and type of hearing loss. Additionally, a tympanometry test may be conducted to assess the condition of the middle ear and the mobility of the eardrum. Surviving your first year with hearing loss can be challenging, but with proper diagnosis and treatment, individuals can learn to effectively manage their condition and communicate successfully.
Weber Test:
- Grasp the tuning fork by its stem and place the stem towards the back of the patient’s head equidistant from either ear. The bones of the skull will transmit this sound to the 8th nerve, which should then be appreciated in both ears equally.
- If there is a conductive deficit (e.g. wax in the external canal), the sound will be heard better in that ear. This is because impaired conduction has prevented any competing sounds from entering the ear via the normal route.
- In a sensorineural abnormality (e.g. an acoustic neuroma, a tumor arising from the 8th CN), the sound will be best heard in the normal ear.
- If sound is heard better in one ear it is described as lateralizing to that side. Otherwise, the Weber test is said to be mid-line.

Rinne Test:
- Place the stem on the mastoid bone and instruct the patient to let you know as soon as they can no longer hear the sound.
- Then place the tines of the still vibrating fork right next to, but not touching, the external canal. They should again be able to hear the sound. This is because transmission of sound through air is always better than through bone.
- This will not be the case if there is a conductive hearing loss which causes bone conduction to be greater than or equal to air.
- If there is a sensorineural abnormality (e.g. medication induced toxicity to the 8th CN), air conduction should still be better then bone as they will both be equally affected by the deficit.


Ear, Nose & Throat Examination:
- Introduction, Wash Hands, Consent,
- General Inspection:
- Hair distribution (PCOS, Hypothyroidism)
- Hair Infestations (nits, lice)
- Oily, sweaty hair (Hyperthyroidism, Acromegaly)
- Thin, Dry Hair (Hypothyroidism)
- Scars
- Skull Deformities (Injuries, Congenital, Cleft Lip)
- High Arch Palate (Marfan’s)
- Skin lesions (SCCs, BCCs)
- Skin Pigmentation (Addison’s, Haemochromatosis, Acanthosis Nigricans in Diab/Cush/PCOS/Acr)
- Skin Scaling (Psoriasis, Autoimmune Disorders)
- Abnormal Facies – (Cushing’s, Acromegaly, Addison’s, Graves Hyperthyroidism, Hashimoto Hypothyroidism, Downs Syndrome, Turner’s Syndrome(Female).)
- Facial Symmetry (Facial Nerve Palsies)
- Facial Muscle Fasciculations
- Eye Inspection (Conjunctival Pallor, Scleral icteris, Conjunctivitis, Discharge, Periorbital Oedema)
- Vital Signs:
- Pulse:
- Tachycardia (Infection)
- Bradycardia (if ↑ICP)
- Blood Pressure:
- Hypertension (if ↑ICP)
- Respiratory Rate:
- Bradypnoea (if ↑ICP)
- Temperature:
- Fever (Infection)
- Pulse:
- Ears:
- External Inspection:
- Redness (Infection)
- Swelling (Gouty Tophi)
- Scars
- Lesions (SCC/BCC)
- Discharge
- Palpation:
- Tug Test (for External Ear Infection)
- Cervical Lymphadenopathy (Infection, Malignancy)
- Otoscopy:
- Explain to the patient that it may feel uncomfortable
- Pull Pinna Back and Upward to straighten the canal
- Examine the Left Ear with the Left hand holding the Otoscope (and vice versa)
- Look for:
- Inflammation of External Ear Canal (Otitis Externa)
- Discharge, Blood, Pus, CSF
- Light Reflex of Tympanic Membrane (Eardrum)
- Inflammation of Eardrum (Otitis Media)
- Bulging of Eardrum (Otitis Media)
- Visible Malleus (Normal)
- Identify Borders (Pars Flaccida, Pars Tensa, Umbo)
- Sclerosis (Chronic Otitis Media)
- Tympanic Membrane Rupture
- Impaction by Ceremun (earwax)
- Hearing:
- Whisper Test – “69 & 100” – Whilst distracting the other ear with your hand.
- Weber’s Test – Lateralising? (Conductive Deafness)
- Rine’s Test – Normally Air Conduction is better than bone conduction.
- External Inspection:
- Nose:
- Visual Inspection:
- Redness (Rosacea, SLE, Acne)
- Enlargement (Rosacea, Acromegaly)
- Skin Lesions (Comedones, BCCs, SCCs)
- Scars, Deformities (Broken Nose)
- Discharge, Pus, Blood (Epistaxis)
- Nasal Deviation
- Nasal Polyps (inflammatory from chronic URTI)
- Septal deformities
- Enlarged, Inflamed Turbinates (URTI)
- Palpation:
- Tenderness
- Swelling
- Deformities
- Block Each nostril & Assess for Obstruction
- Sinuses:
- Press/Percuss over Frontal Sinuses (Tenderness = Sinusitis/Congestion)
- Press/Percuss over Maxillary Sinuses (Tenderness = Sinusitis/Congestion)
- Transilluminate Maxillary Sinuses (Shine otoscope through Maxillae & observe illumination in the mouth)
- Visual Inspection:
- Throat:
- Visual Inspection:
- Hydration
- Central or Peripheral Cyanosis
- Mouth Ulcers (UC/Crohns/SCC/BCC)
- Leukoplakia/Erythroplakia (Smoking – Precancerous)
- Buccal Petechiae (Leukaemias, Bleeding Disorders, DIC, Haemorrhagic Infections)
- Buccal Pigmentation (Addison’s Disease)
- Angular Stomatitis (Microcytic OR Macrocytic Anaemias)
- Atrophic Glossitis (Microcytic OR Macrocytic Anaemias)
- Gum Hyperplasia (AML, Methotrexate)
- Bleeding Gums (AML)
- Dentition & Dead Teeth (CVS Risk Factor)
- High Arched Palate (Marfan’s Syndrome)
- Inflamed, Enlarged Tonsils
- Tonsillar Exudate
- Inflamed Pharynx (URTI)
- “Say Ah” – (Glossopharyngeal & Vagus Nerve Lesions)
- Note any Fetor/Bad Breath (Uraemic, Hepatic, Acetone)
- Palpation:
- Bimanual Palpation for enlarged Parotid Gland (Alcoholism, Sialolithiasis)
- Feeling Tongue & Buccal Mucosa for Lumps/Tenderness/Ulcers
- + Cervical Lymph Node
- Visual Inspection:
Thank patient “that concludes my examination”