Table of Contents
EYE EXAMINATION:
History: – (at least 80% of the diagnosis comes from the history)
- Take a meaningful, focussed history.
- Presenting complaint
- Nature of Presenting complaint:
- 1. Abnormal Vision? (Eg. Flashing lights/blind spot/etc)
- 2. Abnormal Sensation? (Eg. Itching/throbbing/pain)
- 3. Altered Appearance?
- Time course
- Sudden onset/Rapid Onset?
- Duration
- Exacerbating (What makes it worse)
- Relieving (what makes it better)
- Associated (What is it associated with)
- Nature of Presenting complaint:
- Past History
- Meds / allergies
- Eg. Are they diabetic
- Eg. What environmental insults (Eg. Welder)
- Family history
- Social history
Possible Presenting Complaints:
- Abnormal vision
- A) Reduced vision: (NB: If Sudden ➔ Probably Vascular in Origin)
- Central Loss:
- Far/Near/Both
- Peripheral Loss:
- Partial/Total loss
- Eg. Scotoma:
- An area of degenerated visual acuity in one’s field of vision, which is surrounded by a field of normal vision.
- Central Loss:
- A) Reduced vision: (NB: If Sudden ➔ Probably Vascular in Origin)


-
- Hemianopia (bilateral):
- Type of partial blindness where vision is missing in the outer half of both the right and left visual field.
- Usually associated with Optic Chiasm lesions.
- Hemianopia (bilateral):

-
- Impaired Night vision (Ie. “Night Blindness”):
- (a symptom of several eye diseases) – Eg. From Vit.A Deficiency.
- A condition making it difficult or impossible to see in relatively low light.
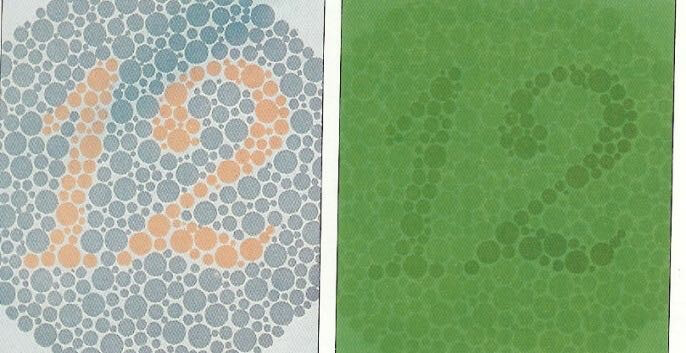
- Colour Blindness:
- 8%males 0.5% females
- (X-Linked Recessive)
- Impaired Night vision (Ie. “Night Blindness”):
- C) Flashers:
- Due to Irritative stimulation of retinal or visual pathway (no sensation)
- Unilateral (retinal)
- Bilateral (Visual Pathway)(Eg. From migraine/basilar artery insufficiency)
- Due to Irritative stimulation of retinal or visual pathway (no sensation)

- D) Haloes
- Rainbow coloured rings around lights
- Due to Diffraction
- Corneal oedema
- Can suggest Increased intraocular pressure
- Rainbow coloured rings around lights

- E) Metamorphopsia / Micropsia:
- Metamorphopsia = Apparent distortion of straight lines
-
- Micropsia = Objects are perceived to be smaller than they actually are
- Possible Causes:
- Retinal oedema ➔ Require urgent referral
- Macular degeneration
-
- Monocular Diplopia:
- Patient sees double when viewing with only one eye.
- Possible Causes:
- Corneal Surface Deformity
- Structural Defect in Eye
- Lesion in Visual Cortex
- Sub-Luxation of Lens
- Monocular Diplopia:

- Abnormal Sensation:
- A) (Stinging/scratching pain) Foreign body sensation:
- Causes include:
- Entropion & Trichiasis (Eyelid folds inward ➔Eyelashes touching cornea)
- Conjunctivitis
- Xerophthalmia (dry eye)
- Can be minimal in IOFB (Intra-Ocular Foreign Body)
- Local anaesthetic relieves it.
- Causes include:
- B) (Achy Pain):
- Eg. Photophobia (excessive sensitivity to light and the aversion to sunlight)
- Eg. Iritis (Inflammation of Iris)
- Eg. Keratitis (Corneal Inflammation)
- C) (Severe Deep Pain):
- Eg. Acute Closed Angle Glaucoma ➔ requires Pupil Constriction to open the Canal of Schlemn.
- Eg. Herpes Zoster infection of the Eye.
- D) Asthenopia (eye strain):
- After intensive use of eyes
- Due to:
- Inadequately corrected refractive error
- Heterophoria (motion of the eyes are not parallel to each other)
- E) Watery eyes / discharge
- Overproduction of tears (ocular irritation/ FB)
- Faulty drainage of tears
- Instability of tears (Tears run down face instead of staying in the eyes ➔Dry Eyes)
- A) (Stinging/scratching pain) Foreign body sensation:
- Altered Appearance
- Proptosis (Eye Dislocation)
- From Orbital Infection, trauma, mass
- Eg thyroid
- Proptosis (Eye Dislocation)

- Ptosis (‘small’ eye)
- CN-III nerve lesions
- Levator abnormalities
- Local lid abnormalities eg infections

- Lid retraction
- Where the lid retracts or moves away from the surface of the eye.

- Lesions
- On lids
- On globe eg pterygium

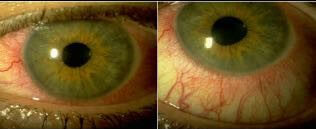
- Diffuse redness
- Ciliary injection
- Corneal/Iris Opacities:

Eye Examination:
- Introduction, Wash Hands, Consent,
- General Inspection of Patient:
- Guide Dog
- Walking Aids
- Visual Aids/Glasses/Eye Patch
- Vital Signs:
- Pulse:
- Particularly Irregularity (AF can ➔ TIAs ➔ Transient Visual Loss “Amaurosis Fugax”)
- Blood Pressure:
- Particularly Hypetension (Hypertensive Retinopathy)
- Respiratory Rate:
- Temperature:
- Fever in Infection
- Pulse:
- Eye Examination:
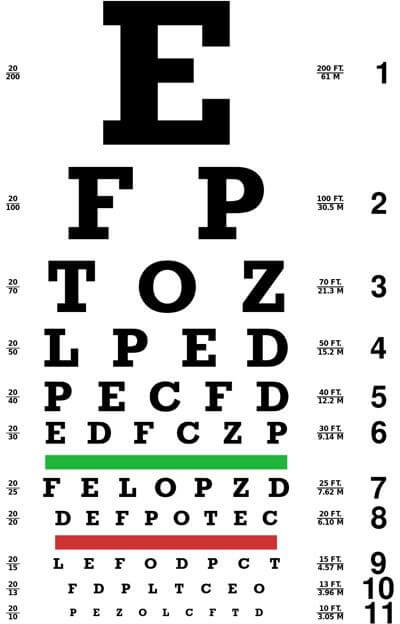
- Visual Acuity:
- Snellens Charts
- Unilateral Corrected + Bilateral Corrected
- If Poor Visual Acuity – Use a Pinhole to see if it is a REFRACTIVE ERROR?
- Blind Spot (Enlarged in Macular Degeneration or Papilloedema)
- Colour Vision:
- Ischihara Charts (Colour Blindness)
- Visual Inspection:
- Eyelids:
- Lid Retraction (Graves Hyperthyroid)
- Lid lag (Graves Hyperthyroid)
- Ptosis (Facial Nerve Palsy, Horner’s Syndrome)
- Periorbital Oedema (Nephrotic Syndrome, Hashimoto Hypothyroidism, Allergies)
- Xanthelasma (Liver Disease, Diabetes, CVD, Cushing’s, Acromegaly, Hypothyroidism)
- Skin Lesions (SCCs, BCCs)
- Eyelashes (Trachoma)
- Eyeball:
- Exophthalmos/Proptosis (Grave’s Hyperthyroid, Leukaemias, Head Injury, Cushing’s)
- Enophthalmos (Horner’s Syndrome, Dehydration)
- Conjunctiva:
- Conjunctival Pallor (Anaemia)
- Scleral Icteris (Liver Disease)
- Subconjunctival Haemorrhages (Extreme Coughing)
- Conjunctivitis (Inflammation + Pus)
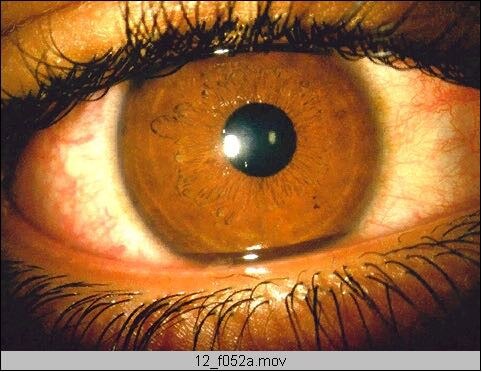
- Iris, Cornea & Lens:
- Arcus Senilis (Sign of CVD Risk factors)
- Copper Ring around the Iris (Wilson’s Disease)
- Horner’s Syndrome (Unilateral Miosis [pinpoint pupils])
- Band Keratopathy (Hypercalcaemia, Hyperparathyroidism, Renal Failure)
- Cataracts (Diabetes, Hypertension, Iodine Deficiency :. Hypothyroidism)
- Corneal Ulceration (Herpes, Trachoma)
- Pus/Blood in Anterior Chamber
- Eyelids:
- Pupil Reactivity To Light:
- Pupil Size (normally 2.5mm-3.5mm)
- Direct Response (If absent = Afferent OR Efferent Nerve Lesion in THAT Eye)
- Consensual Response (If absent = Efferent Nerve Lesion in THAT Eye)
- Marcus-Gunn Pupil (Swinging Torch Test – both pupils should stay the same after a few oscillations due to the Consensual Response) (If one pupil dilates whilst the torch is on the other eye, then that is a Marcus-Gunn Pupil)
- Visual Fields (Remove Glasses & in Confrontation Position + Patient covers one eye):
- Betemporal Hemianopsia = Optic chiasm compression (Pituitary Adenoma)
- Homonymous Hemianopsia = Optic Radiation Lesion
- Unilateral Hemianopsia = Optic Nerve Lesion
- + Blind Spot (If enlarged – May = Macular Degeneration, or Papilloedema)
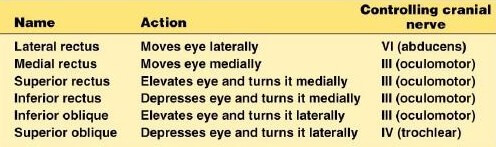
- Extraoccular Movements:
- Occulomotor = Superior Rectus, Medial Rectus, Inferior Rectus, Inferior Oblique
- Trochlear = Superior Oblique (Down & Out) – :. In III-Nerve Palsy, eye faces Down & Out.
- Abducens = Lateral Rectus
- + Nystagmus = Points to the side of a Cerebellar Lesion.
- Fundoscopy:
- Papilloedema
- Macular Degeneration
- Diabetic Retinopathy
- Hypertensive Retinopathy
- Roth’s Spots in Infective Endocarditis.
- Visual Acuity:
“Thankyou, that concludes my Examination”
TESTING THE VISUAL SYSTEM:
- 1. Visual Acuity Tests (Snellen’s Chart):
- All Australian charts are read at 6m (Or are standardised to 6m)
- Tests ‘Corrected’ visual acuity @ a distance. (Those with ‘corrected’ vision use their glasses)
- Each eye is tested Separately; Followed by vision with both eyes open.
- Record results for:
- Right Eye
- Left Eye
- Both Eyes
- The Results are Fraction:
- Numerator = the standardised distance that letter should be read at
- Denominator = The distance that it should be visible from with perfect vision
- Record results for:
- Try using a Pinhole to Improve Visual Acuity (A pinhole eliminates the need for a lens)
- If acuity improves with pinhole, it is a refractive error;
- If acuity doesn’t improve, it is a retinal problem.
- IF they can’t read the snellens chart (even from up close), you need to ask them whether they can see:
- CF (count Fingers)
- HM (Hand movements)
- PL, NPL (Perception of Light/nil perception of light)(Shine a light in their eye)
- IF testing for Presbyopia – use a ‘Near-Reading Chart’.
2. Testing Extraocular Muscles (Eye Movement):
- Start with the target 6inches in front of your partner; Then move your target slowly and smoothly in an wide “H” pattern.
- Look for Conjugate Movement:
- Movement of both eyes in a coordinate manner
- Look for Nystagmus:
- Rhythmic, involuntary oscillation of the eyes.
- Look for Conjugate Movement:
- Is movement Comitant/Incomitant?
- (To the eyes move parallel to each other?)
- (If there’s strabismus, is the same angle of misalignment maintained in all directions?)
- NB: Deviation greatest when move towards field of action of involved muscle.
- Test Convergence for near Vision.

3. Visual field Test:
- Pt stares at your nose.
- A) Testing Peripheral Visual Field: Use your fingers to test vision in peripheries of each quadrant. (Best to use a red-topped bottle/pin)
- Sit in front of Pt with eyes at the same level, about an arm’s length away.
- Cover your left eye.
- Ask your Pt to cover their Right eye and to stare into your open eye.
- Compare your partner’s peripheral visual field to your own:
- Hold up your finger midway between yourself and the Pt (so it is just out of your field of vision).
- Move your finger slowly towards the centre asking the patient when they first see it.
- Test all four quadrants of the visual field (upper right, upper left, lower right, lower left).
- Repeat for the right eye.
- Remember that the visual field and the retina have an inverted and reversed relationship:
- Upper field on the inferior retina
- Lower field on the superior retina
- Nasal field on temporal retina
- Temporal field on nasal retina.

This Diagram is What was Asked in the GLS
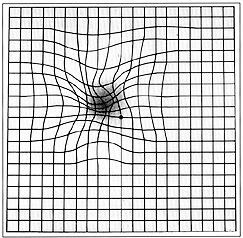
B) Testing Central Visual Field: Use an Amsler Grid to test Pt’s Central Visual Field. (Pts with macular disease may see wavy lines/missing lines) After testing the central visual field with the Amsler Grid, it is important to also conduct an ear, nose & throat examination to assess for any potential issues in those areas that could be impacting the patient’s overall visual health. This comprehensive approach can help us identify any underlying factors that may be contributing to the patient’s visual disturbances and develop an appropriate treatment plan. By addressing both the central visual field and ear, nose & throat health, we can provide thorough care for the patient’s overall well-being.


Normal Eg. Macular Degen.
- 4. Colour vision (Ishihara Tests):
- Tests for colour blindness
- :. Tests Cone Receptors.
- NB: Men are Most Affected by Colour Blindness:
- Because it is Sex-Linked Recessive (on the X-Chromosome), and therefore acts dominantly when inherited in males (who only have 1x X-Chromosome).
- Red-Green photoreceptor disorders are most common.
- People with normal colour vision can see numbers in the pics below:
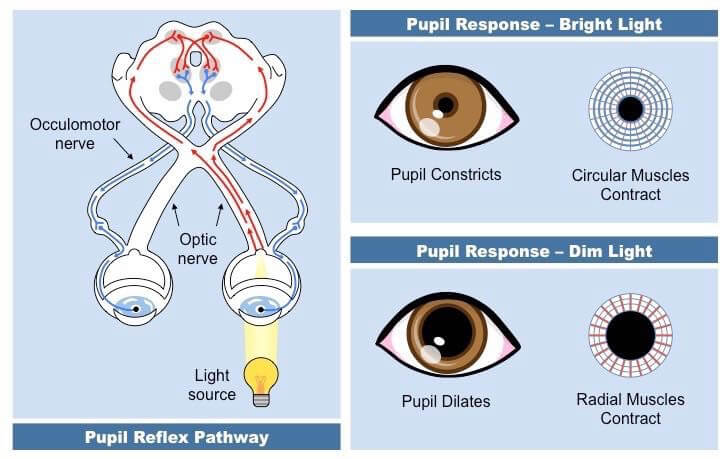
- 5. Pupillary Reflexes:
- (NB: The constriction reflexes are Parasympathetic-Mediated)
- PERLA is Pupils Equal Round Reactive to Light and Accommodation.
- A bright source of light is used to test pupillary reflexes by swinging the light in front of right eye 2 times, while observing 1st right pupil and then the left. Test is then repeated for left eye.
- Dim lights.
- Ask Pt to stare at a target in the distance.
- Turn on the light and look at the right pupil as you swing the light over the right eye. Watch as the pupil constricts.
- This is the direct response.
- Repeat the same procedure again but this time look at the left pupil as you swing the light over the right eye. Does it also constrict?
- This is the consensual response.
- Now repeat the procedure with the left eye. First looks at the left pupil as you shine the light on the left eye, then look at the right pupil.
- Direct:
- Eg. Right Pupil contracts when Right Eye exposed to Light.
- Consensual:
- Eg. Left Pupil Contracts when Right Eye exposed to Light.
- Testing Accommodation-Mediated Pupillary Constriction:
- (Pupil Constriction Associated with the Accommodation)
- Direct:
- Ask your Pt to hold their finger about 8 inches from their nose.
- Ask your Pt to look in the distance and then look at their finger.
- Watch for convergence (crossed eyes) and pupillary constriction.
- NB: Corneal Opacities/Cataracts can Affect the Pupillary Response:
- ➔ Decreased pupillary response in both the affected eye (Direct response) and the other eye (Consensual response) because less light falls on the retina of the affected eye.
- NB: Corneal Opacities/Cataracts can Affect the Pupillary Response:
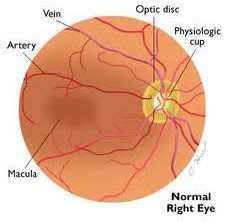
Ophthalmoscopy Technique:
- Ask pt to look straight ahead both eyes open
- Set to zero
- Use right hand and right eye for pt’s right eye, and left ditto for left eye
- Hold sight hole as close as possible to your eye, steady it against your nose
- Gently raise lid with your thumb
- Find red reflex (the reddish-orange reflection from the eye’s retina when using an ophthalmoscope)
- Stand at arms length and focus on the pupillary area with ophthalmoscope
- Should be able to see an uniform orange glow
- This is due to light being reflected from the choroidal vessels
- Look for any opacity in the red reflex
- (Abnormal or absent reflex especially in children could mean sight threatening condition. Need to be referred and treated quickly otherwise vision fails to develop)

- Follow it in at about 15 degrees temporal to line of vision
- Focus
- Find a blood vessel
- Follow it to the disc
- Systematically examine
- Vessels / Macula / Vessels
- Optic Disc
- Colour (normal pink)
- Margins – Well defined
- Cup:Disc Ratio. Normal is less than half of the disc diameter. (If ratio is increased ➔ Probably Glaucoma)
- Retina:
- Look for:
- Haemorrhages/Exudates/New Blood Vessels/Arteries/Veins (Bigger & Darker)
- Common causes of retinal changes:
- Diabetic Retinopathy (leading cause of blindness in <60rys)
- Age Related macular degeneration (Leading cause of blindness in >60yrs)
- Hypertensive retinopathy
- Retinal Artery Occlusion
- Retinal Vein occlusion
- Look for:
- Macula:
- Darker than rest of retina (Due to pigment and thick ganglion cell layer)
- Temporal to the disc
- Centre of macula is the fovea.
- No blood vessels overlying the fovea
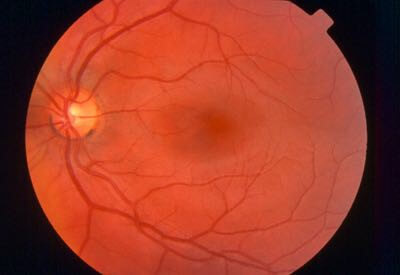
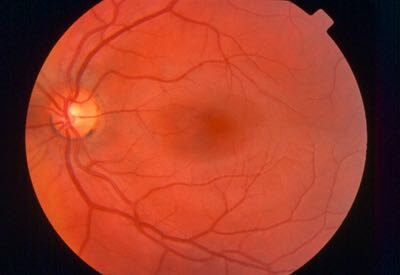
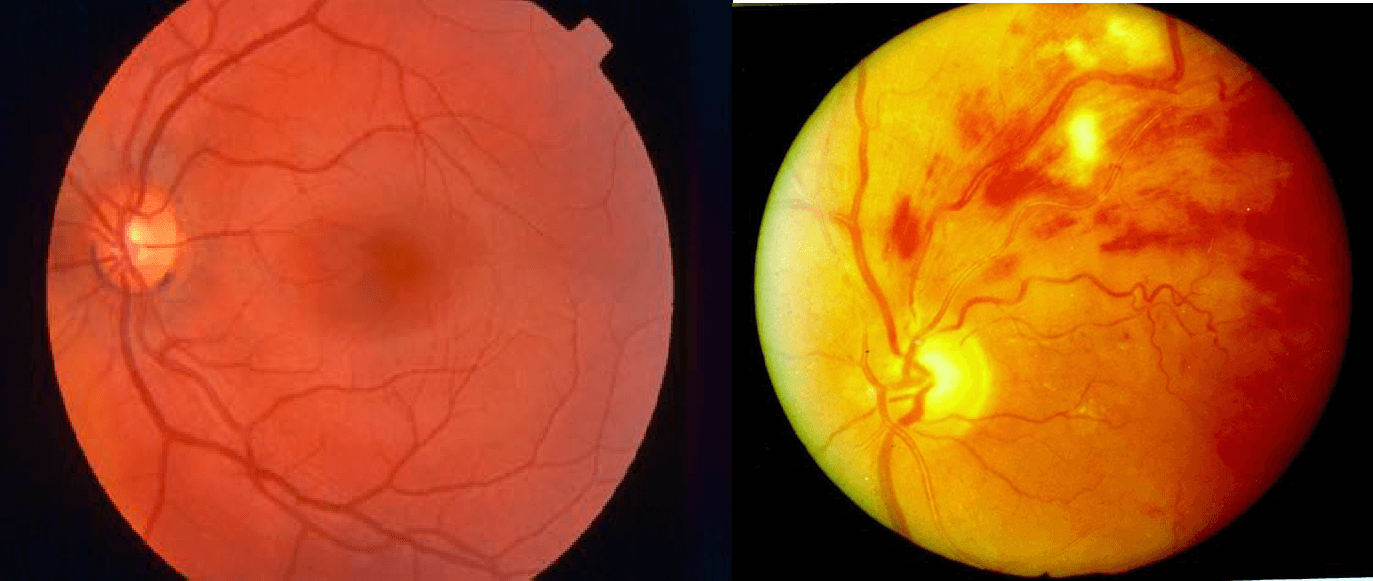
Normal Fundus

ABNORMAL OPTHALMOSCOPY FINDINGS
OPTIC DISC ABNORMALITIES (NORMAL VS. ABNORMAL)
Optic Atrophy
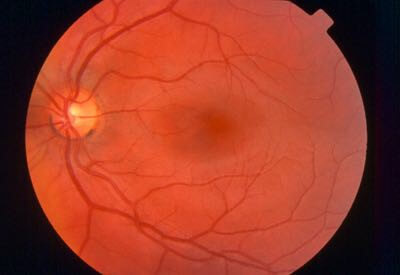
Swollen Disc(Notice disc margin is not well defined)

“Cupping of the Disc”
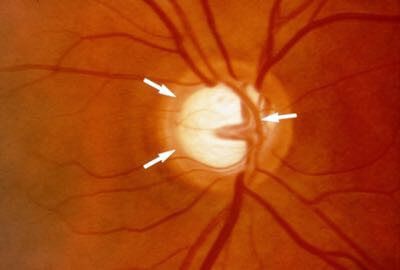
This ratio is approx. 0.6
RETINAL ABNORMALITIES (NORMAL VS. ABNORMAL)
Exudates:

These are soft exudates (Aka: “Cotton wool Spots”) due to ischaemia
BLOOD VESSEL ABNORMALITIES (NORMAL VS. ABNORMAL)
New Vessels (Proliferative Diabetic Retinopathy)


New Vessels (abnormal) – Proliferative diabetic retinopathy (Most common fundal abnormality that you’ll see) These are dangerous because they are very fragile and can bleed very easily. ➔ Impairs Vision
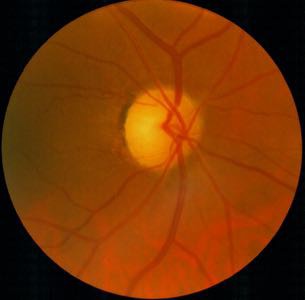
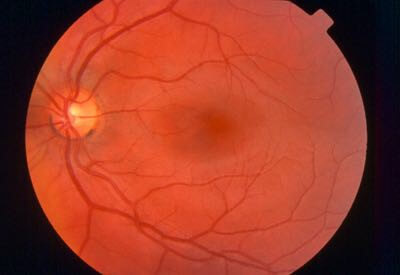
MACULAR ABNORMALITIES (NORMAL Vs. ABNORMAL)
Age Related Macular Degeneration
- Loss of Vision in the Center of the Visual Field (the macula) due to Damage to the Retina.
- ➔Can make it Difficult/Impossible to Read or Recognize Faces, although enough peripheral vision remains to allow other activities of daily life.
- Most common form of blindness in over 65s
Thank You so Much. Happy Learning!!