Table of Contents
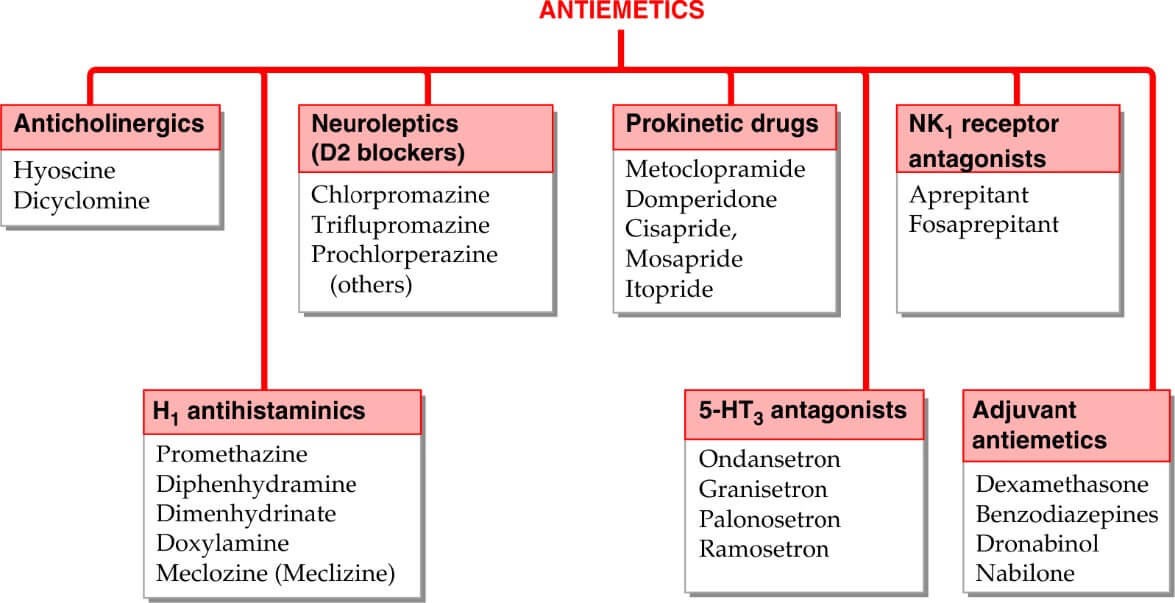
Classification:
|
Drug |
Dosage |
MOA |
ADR |
USES |
|
Ondansetron |
|
motion sickness induced vomiting is not suppressed. |
|
|
Metoclopramide (Prokinetic Drug- promote GI transit and speed gastric emptying by enhancing coordinated propulsive motility)
DOSAGE- 10 mg TDS oral or IM
ACTIONS
GIT
Metoclopramide has more prominent effect on upper g.i.t.; increases gastric peristalsis while relaxing the pylorus and the first part of duodenum → speeds gastric emptying, especially if it was slow. This action is independent of vagal innervation, but is stronger when vagus is intact. Lower esophageal sphincter (LES) tone is increased and gastroesophageal reflux is opposed. It also increases intestinal peristalsis to some extent, but has no significant action on colonic motility and gastric secretion.
CNS
Metoclopramide is an effective antiemetic; acting on the CTZ, blocks apomorphine induced vomiting. The gastrokinetic action may contribute to the antiemetic effect. However, it has no chlorpromazine (CPZ) like antipsychotic property, though it does share the extrapyramidal and prolactin secretion augmenting action of CPZ.
MECHANISM OF ACTION
Metoclopramide acts through both dopaminergic and serotonergic receptors
D2 antagonism
Dopamine (acting through D2 receptors) is an inhibitory transmitter in the g.i.t. — normally acts to delay gastric emptying when food is present in stomach. It also appears to cause gastric dilatation and LES relaxation attending nausea and vomiting. Metoclopramide blocks D2 receptors and has an opposite effect— hastening gastric emptying and enhancing LES tone by augmenting ACh release. However, clinically this action is secondary to that exerted through 5HT4 receptors. The central antidopaminergic (D2) action of metoclopramide on CTZ is clearly responsible for its antiemetic property. Other manifestations of D2 blockade are antagonism of apomorphine induced vomiting, CPZ like extrapyramidal effects and hyperprolactinaemia.
5-HT4 agonism
Metoclopramide acts in the g.i.t. to enhance ACh release from myenteric motor neurones. This results from 5-HT 4 receptor activation on primary afferent neurones (PAN) of the ENS via excitatory interneurons. The gastric hurrying and LES tonic effects are mainly due to this action which is synergised by bethanechol and attenuated by atropine.
5-HT3 antagonism
At high concentrations metoclopramide can block 5-HT3 receptors present on inhibitory myenteric interneurons and in NTS/ CTZ. The peripheral action can augment ACh release in the gut, but appears to be minor. The central anti 5-HT 3 action appears to be significant only when large doses are used to control CINV.
|
ADR |
USES |
|
|
Domperidone
It is a D2 receptor antagonist, chemically related to haloperidol, but pharmacologically related to metoclopramide.
The antiemetic and prokinetic actions have a lower ceiling. Unlike metoclopramide, its prokinetic action is not attenuated by atropine and is based only on D2 receptor blockade in upper g.i.t. Domperidone crosses blood-brain barrier poorly. Accordingly, extrapyramidal side effects are rare, but hyperprolactinemia can occur.
The antiemetic action is exerted mainly through CTZ which is not protected by blood-brain barrier. Because of poor entry into CNS, it does not block the therapeutic effect of levodopa and bromocriptine in Parkinsonism, but counteracts their dose-limiting emetic action.
SIDE EFFECTS
Are much less than with metoclopramide.
Dry mouth, loose stools, headache, rashes, galactorrhoea are generally mild. Cardiac arrhythmias have developed on rapid i.v. injection.
INDICAITIONS
Its indications are similar to that of metoclopramide, but it is a less efficacious gastrokinetic and not useful against highly emetogenic chemotherapy.
DOSE: 10–40 mg (Children 0.3–0.6 mg/kg) TDS