Table of Contents
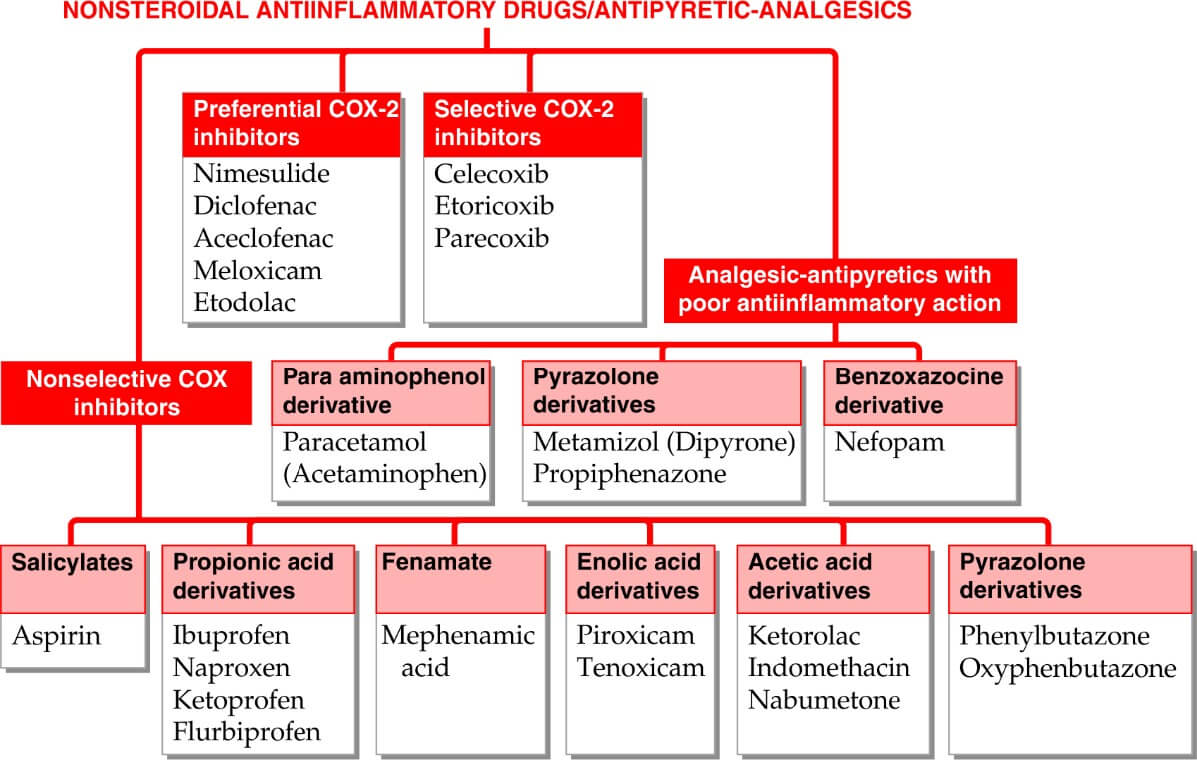
Classification:
COX-1- Constitutive form, serve housekeeping functions
COX-2– Inducible form, inducible by cytokines and other signal molecules at site of inflammation
Non-Selective COX-1/2 vs. Selective COX-2: No antiplatelet aggregatory, gastric mucosal damage, Aspirin sensitive asthma precipitation in selective COX-2 inhibitors
Effects of NSAIDS
|
Analgesics |
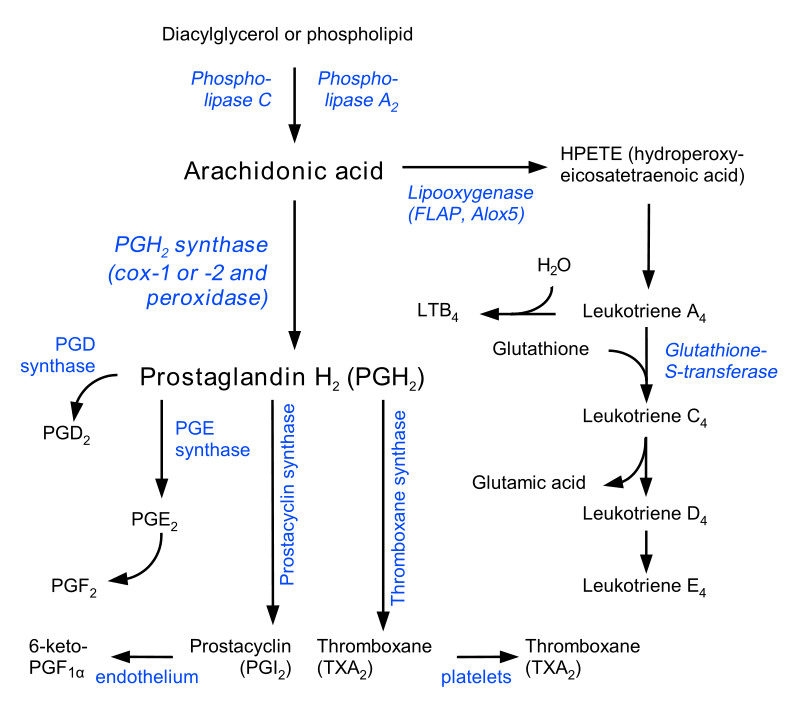
PGs induce hyperalgesia, NSAIDs block pain sensitizing mechanism induced by bradykinin, TNF alpha, IL by primarily inhibiting COX-2 |
|
Antipyretics |
Decrease PGE2- in hypothalamus- decrease set point- reduces fever by promoting heat loss (sweating, cutaneous vasodilation but does not decrease heat production), COX-2 mediated |
|
Anti- inflammatory |
Inhibition of COX-2 mediated suppression of PGs. |
|
Antiplatelet aggegatory |
Inhibit synthesis of TXA2 which is proaggregatory, COX-1 mediated |
|
Ductus arteriosus closure |
PGE2 inhibition ,COX-2 mediated, if NSAID given in pregnancy premature closure occurs, so avoid NSAIDs near term |
|
Labor |
Delay labor due to inhibition of PGs |
|
Gastric mucosa damage |
Inhibit COX-1 mediated protective PGs synthesis, decreased bicarbonate secretion, enhance acid secretion |
|
Renal effect |
In hypovolemia, decreased renal perfusion and Sodium loss-> PGs-> vasodilation, NSAIDs can:
|
|
Dysmenorrhea |
In dysmenorrhea, PG elevated, NSAID lower uterine level of PG- Provide relief |
|
Anaphylactoid reactions |
Precipitate asthma, Angioneurotic swellings, urticarial: Immunologically mediated |
Salicylates (Aspirin- Prototype)
MOA AND OTHER ACTIONS
- Acetylation of COX
- Analgesic, antipyretic, anti-inflammatory action– Weaker analgesic than morphine; good anti-inflammatory action; anti-inflammatory action at high dose
- Metabolic effect– cellular metabolism increased, esp. in skeletal muscle due to uncoupling of oxidative phosphorylation-> increase heat production; increased utilization of glucose-> blood sugar may deplete; liver glycogen is depleted; hyperglycemia at higher dose due to sympathetic stimulation
- Respiration- dose dependent, at anti-inflammatory dose respiration is stimulated by peripheral as well as central action- Hyperventilation; further increase in salicylate level causes respiratory depression causing death
- Acid-base and electrolyte balance- usual analgesic dose has no effect; anti-inflammatory doses produce significant change in AB balance and electrolyte composition; initially respiratory stimulation-> CO2 wash out-> respiratory alkalosis; which is compensated by renal excretion of HCO3– with accompanying Na+, K+ and water; still higher dose cause respiratory depression-> CO2 retention-> respiratory acidosis; dehydration occur in poisoning due to water loss in urine
- Gastric mucosa damage- Inhibit COX-1 mediated protective PGs synthesis, decreased bicarbonate secretion, enhance acid secretion
- GIT- aspirin and released salicylic acid irritates gastric mucosa-> causes epigastric distress, N, V, stimulates CTZ: vomiting; aspirin remains unionized and diffusible in gastric juice but on entering mucosal cell it ionizes and becomes in diffusible; this ion trapping in gastric mucosal cell enhances gastric toxicity further aspirin particle coming in contact with gastric mucosa promote local back diffusion of acid-> focal necrosis of mucosal cells-> acute ulcers, erosive gastritis, congestion and microscopic hemorrhages
- Urate excretion- retention at low dose and increased excretion at high dose
- Blood- Aspirin even in small doses, irreversibly inhibits TXA2 synthesis by platelets. Thus it interfere with platelet aggregation and bleeding time is prolonged to nearly twice the normal value. This effect lasts for about a week (turnover time of platelet); long term intake of large dose decrease synthesis of clotting factors in liver and predisposes to bleeding; prevented by giving prophylactic vit K
ADVERSE EFFECTS
|
Side effects- at analgesic dose |
N, V, Epigastric distress, increased occult blood in stool, gastric mucosal alteration and peptic ulcer |
|
Hypersensitivity and idiosyncrasy |
Rashes, FDE, Urticaria, Rhinorrhea, Asthma, Anaphylactoid reaction |
|
Anti-inflammatory dose (3-5 g/day) |
Salicylism- Dizziness, tinnitus, vertigo, reversible impairment of hearing and vision, excitement, hyperventilation Children with RA- Liver damage Children with viral infection- influenza, varicella- Reye’s syndrome- a rare form of hepatic encephalopathy |
|
Acute salicylate poisoning |
At fatal dose– Vomiting, diarrhea, acidotic breath, hyper/ hypoglycemia, restlessness, delirium, hyperpyrexia, convulsion, coma and death due to RF+ CVS collapse Treatment– Symptomatic and supportive, Gastric lavage, IV fluids with Na, K, HCO3, Glucose |
CONTRAINDICATIONS
- Aspirin sensitivity
- Peptic ulcer
- Bleeding tendency
- Chicken pox, influenza
- Diabetics
- CLD- can cause hepatic necrosis
- 1 week before surgery
- 3rd trimester- can cause prolonged labor, premature closure of DA
- G6PD- can cause hemolysis
USES
- Analgesic– headache, backache, myalgia, joint pain, pulled muscle , toothache, neuralgia, dysmenorrhea
- Antipyretics– PCM is safer
- Acute rheumatic fever
- Rheumatoid arthritis
- Osteoarthritis
- Post myocardial infarction and Post stroke Pts.
- Patent ductus arteriosus
| Drug s |
Dosage |
MOA |
ADR |
USES |
|
Paracetamol (acetaminophen) |
|
|
Acute PCM poisoning
|
|
|
Ketorolac |
|
mechanism |
|
|
|
Ibuprofen |
|
|
|
|
|
Nimesulide |
|
|
|
|